There are a lot of bacteria out there. As in, a lot a lot. There may be more than 5 nonillion (that’s 1030) bacteria on Earth. A single milliliter of fresh water typically holds around one million bacterial cells. About 30,000 species of bacteria have been named, and there may be more than a billion species waiting to be identified. Even in your own body, about 10% of your body weight is due to bacteria, including some that need to be present for you to stay healthy.

We’ve only identified a small fraction of the billions of bacterial species that exist on Earth.
©bogdanhoda/Shutterstock.com
As you can imagine, it’s challenging to get a handle on all these bacterial species. One tool that helps scientists identify bacteria, first developed nearly 140 years ago, is called Gram staining. And amazingly, this technique—developed in a Berlin morgue as bacteriology was just starting to come into its own as a science—is still one of the most commonly performed tests in clinical microbiology labs today.
How to See the Invisible
Some types of bacteria may have been seen with the first microscope observations in 1683. But it wasn’t until the late 19th century that the science of bacteriology really got cooking. That’s when researchers began carefully observing and describing the various shapes and structures of bacteria. It’s also when Louis Pasteur and others established a link between bacteria and disease.
One problem with studying bacteria: they’re hard to see. Not only are they so small that a microscope is required, bacterial cells have very little natural pigment. As a result there’s little contrast between the transparent bacterium and its environment. So early on, researchers learned to add dyes that would stain bacteria and other microbial life forms, as well as some of their internal structures. As microscopes became more sophisticated, so did staining techniques.
Meet Hans Christian Gram
In 1884, with new discoveries by Pasteur and other researchers revealing the medical importance of bacteria, a Danish scientist named Hans Christian Gram was trying to isolate the cause of bacterial pneumonia. While working at the city morgue, Gram examined lung tissue samples. He noticed that when a common stain was applied, and then washed away with ethanol, some bacteria held on to the stain while others didn’t. In a series of experiments, Gram found that certain types of bacteria remained stained after a solvent was applied. Others lost the coloration. This meant that the staining technique could not only make bacteria more visible, it could distinguish some kinds of bacteria from other kinds. Gram published his findings, and the Gram staining technique has been in use ever since.
How Does Gram Staining Work?
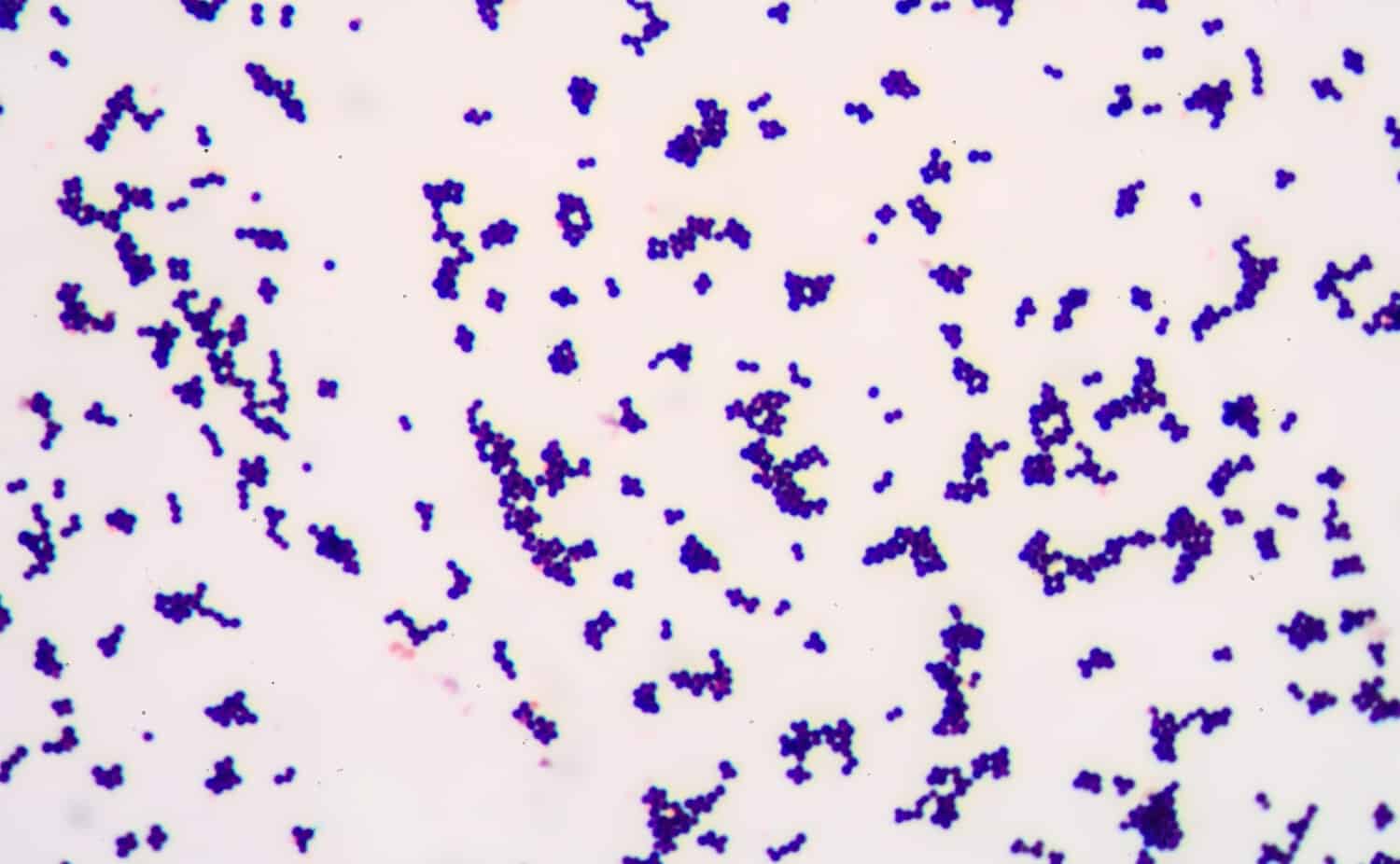
Gram-positive bacteria retain a purple or blue color after staining.
©Schira/Shutterstock.com
Gram staining is performed in a laboratory on a tissue sample taken from the site of a suspected bacterial infection. The sample might be collected by swabbing a part of the body, like the throat or skin, or by collecting a bodily fluid like spit or urine. Sometimes fluid from inside the body is removed with an aspirating needle. In a medical laboratory, the sample is placed on slides for staining.
Bacteria that are stained by the Gram test are called Gram-positive bacteria. Those that are not stained are called Gram-negative bacteria. In a final step that’s been added to Gram’s original process, a second stain is added. This gives Gram-negative bacteria a different color. So Gram-positive bacteria are typically stained purple or blue, while Gram-negative bacteria turn pink or red.
Positive or Negative
The reason bacteria react differently to Gram staining is because of the organisms’ cell walls. The cell wall is a specialized protective layer surrounding the bacterial cell. (Plant cells also have cell walls, but animal cells do not.) Gram-negative bacteria have a thin cell wall that the solvent in the Gram process can easily penetrate. So they lose the staining color. Gram-positive bacteria have a thick wall that the solvent can’t penetrate, so they stay stained.
The Gram stain helps doctors categorize what type of bacteria are present in an infection, both by the presence or absence of the coloration, and by the shape of the bacteria revealed by the stain.
Some common Gram-negative bacteria include:
| Bacteria | Condition it causes |
| E. coli | Food poisoning, urinary tract infection |
| Salmonella | Food poisoning |
| M. morganii | Sepsis, pneumonia, wound infection |
| L. pneumoniae | Legionnaire’s disease |
| Aeromonas | Eye infection, meningitis |
Some common Gram-positive bacteria include:
| Bacteria | Condition it causes |
| S. pneumoniae | Bacterial pneumonia |
| Streptococcus group A | Strep throat |
| Listeria | Food poisoning |
| C. botulinum | Botulism |
| S. aureus | Toxic shock syndrome, MRSA |
Limitations of Gram Staining
Gram stains don’t usually diagnose the specific bacteria causing an infection, but they point healthcare providers in the right direction. As a quick and easy lab test, it tends to be the first step in identifying bacteria. When needed, more specific procedures can follow, to zero in on a bacterial culprit. Gram staining can’t detect some types of bacteria, so alternate tests need to be used.
The photo featured at the top of this post is © iStock.com/Md Saiful Islam Khan
Thank you for reading! Have some feedback for us? Contact the AZ Animals editorial team.